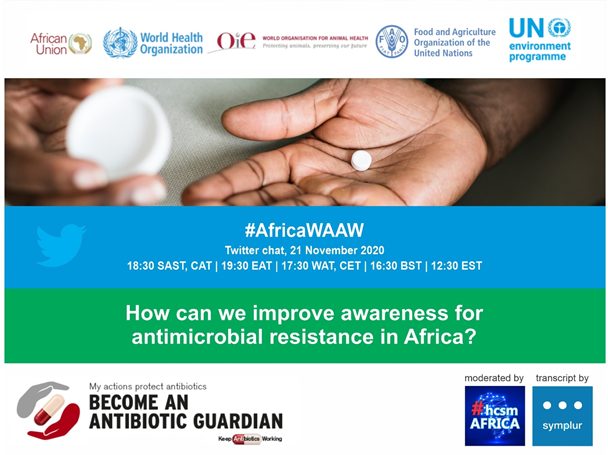
Date: Saturday, 21 November 2020
Time: 18:30 SAST, CAT | 19:30 EAT | 17:30 WAT, CET | 16:30 BST | 12:30 EST
Hashtag: #AfricaWAAW
Moderator: @hcsmAFRICA (Vanessa Carter)
Join us for a 60-minute Twitter chat to share your views about how we can increase awareness for antimicrobial resistance in Africa. All stakeholders including healthcare professionals, civil society, policymakers, journalists, nurses, medical researchers, IT experts, veterinarians, pharma, students etc. locally and globally are welcome. The public transcript will be recorded by Symplur.
To participate, use the hashtag #AfricaWAAW
QUESTIONS:
T1: Why is it important to improve awareness about antimicrobial resistance in Africa?
T2: Which stakeholders matter in controlling antimicrobial resistance?
T3: How do you think we can improve awareness of antimicrobial resistance among all stakeholders?
T4. What barriers make it difficult to improve awareness about antimicrobial resistance in Africa?
T5: How would you describe antimicrobial resistance to others? (e.g. another language, or plain language)
CT: Do you have anything you want to add about antimicrobial resistance awareness in Africa?
TOPIC:
During this 1-hour Twitter chat, the Africa Union, Africa Regional Tripartite (FAO, OIE and WHO) and UNEP want to hear your thoughts about how we can increase awareness for antimicrobial resistance in Africa.
How can we increase awareness for antimicrobial resistance in Africa?
World Antimicrobial Awareness Week (WAAW) which takes place between 18 – 24 November 2020 aims to increase awareness of global antimicrobial resistance (AMR) and to encourage best practices among the general public, health workers and policy makers to avoid the further emergence and spread of drug-resistant infections.
What are antimicrobials?
Antimicrobial medicines are different types of drugs that can be grouped according to the microorganisms they treat. For example, antifungals kill fungi, antibiotics are used for bacteria, antivirals treat viruses and antiparasitic drugs kill parasites. We rely on these medicines for a wide range of conditions and diseases including for cancer treatment, to prevent infections after routine surgery or more extensive procedures like organ transplants, prevent and treat malaria and other types of zoonotic diseases such as Lyme disease which is caused by tick bites, listeria found in food products like unpasteurized milk or sandwich-meat, in dentistry, for urinary tract infections, some respiratory infections like pneumonia or TB as well as for sexually-transmitted infections, HIV/AIDS, and maternal and newborn health. Since the first antibiotic drug class called Penicillin was discovered in 1928 by Sir Alexander Flemming, antimicrobial drugs have saved billions of lives and are the cornerstone of modern medicine.
What is causing antimicrobial resistance?
Antimicrobial Resistance occurs naturally over time and most often through genetic changes. Most microorganisms have used their survival mechanisms (genetic changes) to resist the effect of antimicrobials. Since the discovery of these miracle antimicrobial drugs, overuse and misuse in the human, animal and environmental health sectors as well as agriculture have led to an increase (upsurge) in the selection pressure leading to resistance. An example of misuse is when a specific class of antimicrobials know as an antibiotic is prescribed for the common cold or flu while the flu or the common cold are not caused by bacteria but rather viruses. Antibiotics are only effective at treating bacterial infections therefore in this case we end up taking them unnecessarily. In the animal sector, antimicrobial drugs are being misused for various purposes including growth-promotion, a practice used to increase weight gain of animals and not to treat diseases. The natural phenomenon of microbial adaptation to survive antimicrobials, enhanced by the overuse or misuse of antimicrobial drugs is known as antimicrobial resistance and the microorganisms that become resistant are called “Superbugs”.
What types of superbugs should we be worried about?
An example of a superbug commonly found in hospital settings, as well as in the community and in livestock is Methicillin-resistant Staphylococcus aureus (MRSA). Staphylococcus aureus is a common type of bacteria that lives on our skin and on mucosal surfaces such as our noses, even in healthy people, but when Staphylococcus aureus develops resistance against a type of antibiotic called Methicillin, that drug will no longer be effective in treating it. There are countless more types of superbugs including drug-resistant tuberculosis, drug-resistant typhoid fever, Clostridium difficile (C.diff) and Carbapenem-resistant Acinetobacter baumannii (CRAB), a type of bacteria commonly found in the environment, especially in soil and water.
How can we slow down antimicrobial resistance?
Microbes are part of nature and live all around us, some of them even live harmoniously inside our body, but every now and again a bad one can cause an infection or disease. One of the most important things we can do besides reducing the overuse and misuse of antimicrobial medicines is to practice good hand hygiene. The COVID-19 pandemic highlights some important lessons around infection prevention and control (IPC), one of which was handwashing to reduce the spread of the virus. That same principle should be used as we tackle the spread of deadly superbugs. Self-medicating or sharing antimicrobials like antibiotics with others without the guidance of a qualified medical professional can also put the user at a higher risk of developing resistance and at some point, when their life depends on those drugs, they might not work. Understanding that different antimicrobial drugs treat different types of microorganisms help us understand why a particular type of drug like an antibiotic was not prescribed. This is why it is critical to seek the advice of a qualified health professional before using antimicrobials. The same goes for caretakers of livestock and companion animals seeking advice of an animal health professional before using antimicrobials as well as never borrowing antibiotics from other animal owners.
Education is empowering, but is it enough to change behaviour?
There are numerous actions we can all take to tackle antimicrobial resistance if we are informed to make the right decisions, not only for ourselves and families but also for the community these dangerous superbugs can spread to. One of the barriers to achieving education in Africa is effective health communication because antimicrobial resistance can be a difficult concept to describe where some African languages don’t have the technical terms to explain it, or otherwise where health literacy barriers mean that plain language is necessary. Beyond education, there are also certain choices that we can make as an individual because we want to be part of the solution. Let us do whatever we can to keep these precious antimicrobial medicines working, because without them we risk going back to an era where a simple infected cut can become fatal.
Join World Antimicrobial Awareness Week 2020 Campaign for Africa events from 18 – 24 November 2020.
FURTHER READING:
- Africa CDC Framework for Antimicrobial Resistance in Africa 2018- 2023
- WHO Global Action Plan on Antimicrobial Resistance
- FAO Global Action Plan on Antimicrobial Resistance
- UNEP report – Antimicrobial Resistance: Investigating the Environmental Dimension
- The OIE Strategy on Antimicrobial Resistance and Prudent Use of Antimicrobials

- Chats are public. Even if you use a platform like tchat.io, they still show on your timeline. Think before you tweet! Read more about maintaining a good digital footprint here.
- Please respect other members of the community and show courtesy at all times.
Refer to the Twitter Terms and Conditions of use. Disrespectful behaviour can be reported. - Don’t be afraid to lurk, although participation is always encouraged, even if the topic is not within your expertise, your voice matters.
- Visit www.symplur.com to check out the analytics and transcript which is open to the public.
- If you don’t understand a question from the moderator, don’t be afraid to speak up and ask for clarity.
- Use this opportunity to network with other stakeholders and follow them on Twitter.
- When entering the Twitter chat, first introduce yourself and tell other members what you do so they get to know you.
- If you agree with a member’s perspective in a chat, go ahead and retweet them to show you support their idea.
- The chat runs for 60 minutes, but you can join in at any time.
- Start answers with the relevant T’s and number for transcript purposes.
- Answer each question after the moderator prompts but keep answers coming even if we move onto the next one. We don’t want to miss out on your views!
- Both panel experts and public attendees are invited to participate.
- Use the hashtag #AfricaWAAW in all tweets or you won’t be visible in the chat.
- More information about how to participate in a Twitter chat can be read here
TWEETCHAT GUESTLIST
- Anna Dumitriu, Artist-in-Residence Modernising Medical Microbiology – University of Oxford, and The National Collection of Type Cultures – Public Health England – @AnnaDumitriu
- Dr Wendy Thompson, Dental Antibiotics, FDI World Dental Federation – @WendyTheDentist
- Tochi Okwor, Nigeria Centre for Disease Control – @tokwor7
- Dr Abiodun Egwuenu, AMR Programme Manager, NCDC -@beeodune
- Dr Walter Fuller, Technical Officer for AMR, WHO AFRO –
- Sien Ombelet, Academic Assistant at Institute of Tropical Medicine in Antwerp (ITM) -@SOmbelet
- Esteller Mbadiwe – Founding Partner Ducit Blue Solutions, Clinical Governance Advocate, Antimicrobial Guardian – @Onyi_Estelle
- Dr Mirfin Mpundu, Director of ReAct Africa – @MirfinM
- Niniola Williams, Managing Director of DRASA (Dr. Ameyo Stella Adadevoh) Health Trust – @drasatrust
- Dr Scott Newman, Food and Agriculture Organization – @scottnewmanfao
- Ki Min, FAO Africa AMR Communications Specialist – @kijung_min
- Dr Haileyesus Getahun -Dr Haileyesus Getahun, Director, Global Coordination and Partnership (GCP) on Antimicrobial Resistance, World Health Organization – @hygetahun
- Students Against Superbugs Africa is a student-driven initiative which seeks to empower young people to be active advocates in the fight against Antimicrobial Resistance – @beat_the_bugs
- Chioma Achi, Doctoral Researcher at the University of Cambridge – @Chijev
- Dr Diane Ashiru-Oredope, Lead Antibiotic Guardian Campaign, Lead Pharmacist HCAI & AMR Division, Public Health England. @DrDianeAshiru
- Dr Shakira Choonara, African Union Youth Council – @ChoonaraShakira
- Professor Iruka N Okeke, University of Ibadan – @iruka_okeke
- Professor Sabiha Yusuf Essack, South African Research Chair in Antibiotic Resistance and One Health, Global Hygiene Council – @EssackSabiha
- Otridah Kaponar, Public Health Laboratory Scientist/ Antimicrobial Resistance National Focal Point & Coordinator Zambia – @OttyKaps
- Stephanie Salyer, Technical Advisor to Africa CDC, Addis Ababa, Ethiopia – @Steph_Salyer
- Dr Justin M. Maeda, Head of Surveillance and Disease Intelligence, Africa Centres for Disease Control and Prevention -@JustinMMaeda
- Tumaini MAKOLE, Pharmacist | Public Health Advocate | AMR | Health Technology Enthusiast, Tanzania – @TumainiMakole
- Stan Ibeanu, Federal Ministry of Agriculture & Rural Development, Nigeria -@Stanarizona
- Kalema Musisi Solomon, Senior Knowledge Management Officer at Ministry of Agriculture, Animal Industry and Fisheries, Uganda – @solomonkalema1
- Chidubem Okonkwo, Environmentalist, Nigeria – @CDubem_
- Lloyd Phillips, Senior agricultural journalist – Farmer’s Weekly South Africa – @PhillipsLM
- Leventis Foundation – @LeventisAgriSch
- Nigeria Health Watch, Nigeria Health Watch uses informed advocacy and communication to influence health policy and seek better health and access to healthcare in Nigeria – @nighealthwatch
- Dr Pascale Ondoa, African Society for Laboratory Medicines (ASLM)
- Benjamin Park, Elizabeth Bancroft, Joyce E. Thomas, US CDC – @CDC_NCEZID
- HAMZAT, Omotayo Tirimidhi – @hamzatTayo
- OUSMAN, Kevin Babila – Technical Officer, Infection Prevention and Control Emergency Preparedness and Response WHO Regional Office for Africa – @kousman
- Jane Lwoyero, Programme officer AMR at the OIE – @JaneLwoyero
- Patrick Bastiaensen, Programme Officer at the OIE – @furrysentinel
- Olafur Valsson, Programme Officer AMR at the OIE – @OValsson
- Pidemnewe Pato, Programme Officer OIE – @pidemnewe
- Brice Lafia, Programme officer OIE – @brice_lafia
- Taylor Gabourie, Communications Officer AMR – @tagabourie
- Dr Olga Perovic, Associate Professor, Pathologist at the National Institute of Communicable Diseases South Africa – @Puseletso
- Mark Rweyemamu, SACIDS
- Lolo Nomsu, Public Health Officer – @Nomsu__
- Dr. Dishon Muloi , International Livestock Research Institute (IRLI) – @dishonmuloi
- Jeremy Knoxx, Policy and Advocacy Lead for Antimicrobial Resistance at the Wellcome Trust – @_Jeremy_Knox
- David Mpaju, Makerere University, Former MUMSA president, winner of innovative 4AMR and voices of diagnosis. @MpajuD
- Francesca Chiara, The Surveillance and Epidemiology of Drug-resistant Infections Consortium (SEDRIC) – @FrancyChiara_
- Dr Zawaira, Assistant Regional Director (ARD) WHO-AFRO – @ZawairaFelly
- Diriba Agegnehu Mosissa, WHO AFRO – @DiribaMosissa
- Moses B. Bolongei, Public Health Specialist, WHO AFRO – @bolongei_moses
- Jessica Craig and Erta Kalanxhi, Center for Disease Dynamics, Economics & Policy (CDDEP) – @CDDEP
- Prof Philip B. Adongo, President, Association of Schools of Public Health in Africa (ASPHA)
Vice President, World Federation of Academic Institutions for Global Health (WFAIGH) - Wande Alimi AMR Programme Coordinator Africa CDC, Addis Ababa, Ethiopia – @Wande_A