The 12th Annual Conference of Speakers of National and Regional Parliament hosted by the Pan African Parliament (PAP) in Midrand, South Africa, was a landmark event, that brought together Africa’s parliamentarians to shape the continent’s future, discussing key issues on the continent including devastating floods, climate change, Mpox, Non-Communicable Diseases, food security, regional cooperation and peacebuilding.
On 18 September 2024, Dr. Jean Kaseya, Director General of Africa CDC, took to the stage and shared Africa CDC’s vision for a safer and healthier Africa through a speech delivered on his behalf by Dr. Lul Riek, Regional Director for the Southern Africa Regional Coordinating Center. He informed the speakers why the New Public Health Order matters for the continent and how Africa CDC has so far effectively responded to the outbreaks ravaging the continent, including Mpox.
The New Public Health Order is a path towards self-reliance, he said. Existing global mechanisms, policies, and interventions have consistently failed in addressing Africa’s health security priorities, as recently highlighted by the COVID-19 pandemic, Mpox, and Ebola, he told the gathering.
There is a need for a fundamental paradigm shift toward an equitable and just public health landscape through a New Public Health Order for the continent, he explained. The continent must take control of its health security through strong local leadership, innovation, and investment in public health infrastructure and systems, he added.
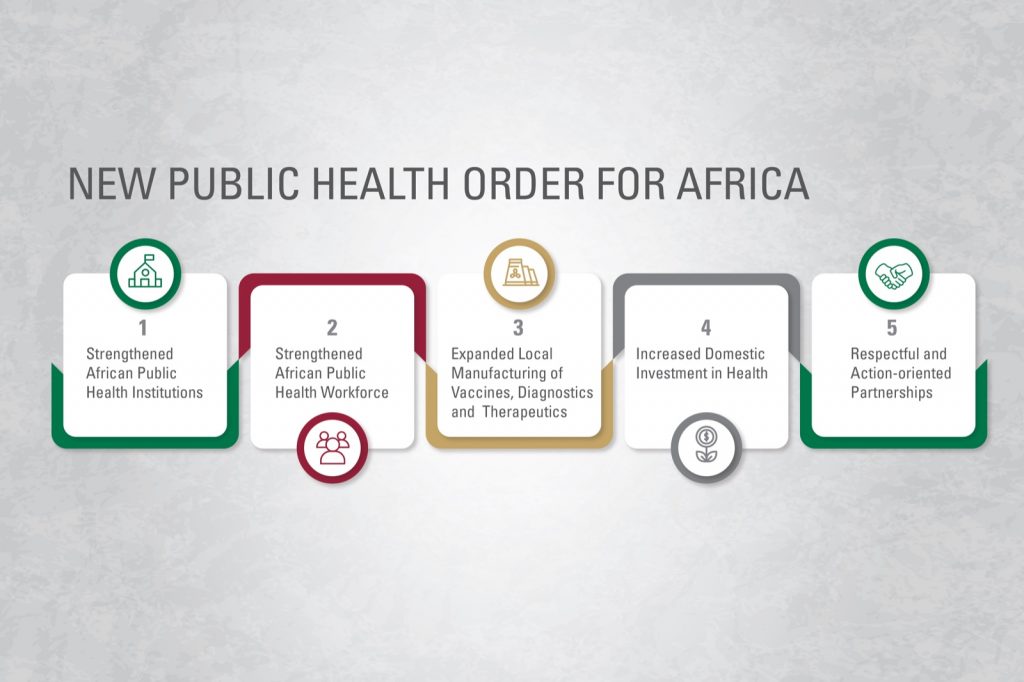
The New Public Health Order aims to ensure adequate health systems exist before a crisis and remain resilient during and post-crisis, he said. Plans to realize this order place an emphasis on the five enablers: community health, connectivity through digital health tools, capacity, collaboration, and climate.
The New Public Health Order envisages strengthened National Public Health and Research Institutes, working with local universities, providing expertise in Emergency Operating Centres (EOCs) and genomic sequencing capabilities. It is geared to develop and expand local manufacturing that will see vaccines, diagnostics, therapeutics, and medical supplies all manufactured from the continent. There is a need for respectful action-oriented partnerships that will ensure long-term engagement, alignment on priorities by African countries with Member States in the driver’s seat.
He said increased domestic health financing should adhere to the Abuja declaration of 2001, which says African countries should allocate 15% of their budgets to health, and respect the ALM declaration, which came in February 2019, when the African Union convened Heads of States and Government and regional and global leaders in Addis Ababa, for the African Leadership Meeting – Investing in Health. The ALM aims to put in place the political and technical mechanisms that will assist and enable countries to steadily increase domestic investment in health year after year and hold each other accountable in the collective commitment to do so. African heads of state also agreed to create the Africa Epidemics Fund in February 2022. The fund can also accelerate the operationalization of the New Public Health Order.
When it comes to a strengthened public health workforce, the New Public Health Order, Dr. Kaseya said, will see the training of more field epidemiologists, the deployment of community health workers, and the training of a new generation of public health leaders, among other health professions, such as the Kofi Annan Fellowship in Public Health Leadership launched on 25th May 2020.
Dr. Kaseya emphasized that the New Public Health Order is grounded in analyses of Africa’s public health systems and institutions. He said 23 Member States have established National Public Health Institutes, but not all are fully operationalized and functioning, and 21 countries are in the process of establishing NPHIs.
Many Member States still rely on indicator-based surveillance systems with limited implementation of event-based or advanced processes, he said. The over 160 disease outbreaks reported annually have revealed gaps in Member States’ abilities to prepare for and respond to emergencies. For instance, only 5 percent of laboratories are equipped to diagnose priority diseases in their countries and meet international standards. Africa relies heavily on imports; only 1% of vaccines and 30-40% of therapeutics are manufactured on the continent. Dr. Kaseya told the parliamentarians that a new 106 events were reported in 2024, and an average of 27 events are monitored weekly: with 3 new events weekly.
As Mpox cases in Africa have surged due to increased human-to-human transmission and insufficient response capacities, he said, key challenges include weak surveillance, limited laboratory capacity, infection prevention practices, public awareness, lack of community engagement, vaccines, and treatments.
Consultations and communication between Africa CDC, WHO, and all the partners led to the establishment of one plan with one team, one rapport, one budget, and one monitoring and evaluation framework. “It’s the first time the agencies are using one continental coordination team, response plan, budget, and monitoring and evaluation framework in a major health response,” he said.
Africa CDC is coordinating with partners to identify and shortlist Mpox testing solutions, including point-of-care test kits. The AU health agency has so far delivered sequencing equipment and reagents to Burundi and the Central Africa Republic, and an automated liquid handling system to speed up testing and sequencing at INRB in DRC. Dr. Kaseya urged the Pan African Parliament and all key stakeholders to support countries to strengthen surveillance, screening at points of entry, awareness, and vaccination campaigns on Mpox.