Monkeypox is a rare viral zoonotic disease caused by a double stranded DNA virus that belongs to the Orthopoxvirus genus of the Poxviridae family. The disease presents with symptoms similar to smallpox but with a lesser severity.
Monkeypox was first discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research, hence the name ‘monkeypox.’ The first human case of monkeypox was recorded in 1970 in the Democratic Republic of the Congo (DRC), which has subsequently spread to other central and western African countries. There are two known clades of the virus: clade I and clade II. The clade I, which is most frequently reported from countries in central Africa, tends to be more severe than clade II. Cameroon is the only country known to harbour both clades.
Key Facts
What
Where
Transmission
Symptoms
Recovery
Testing
Vaccines
Frequently Asked Questions
Mpox, formerly known as monkeypox, is a rare viral zoonotic disease caused by the monkeypox virus. It is primarily found in tropical rainforest areas of Central and West Africa and presents with symptoms similar to smallpox, though generally less severe. The virus has two distinct clades: Clade I and Clade II.
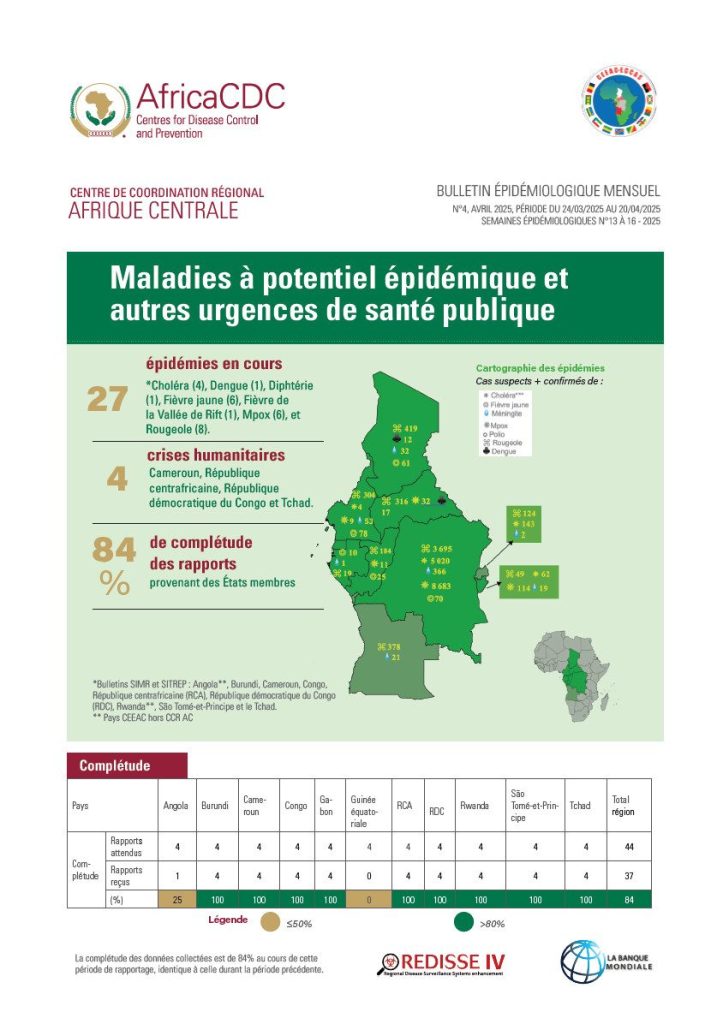
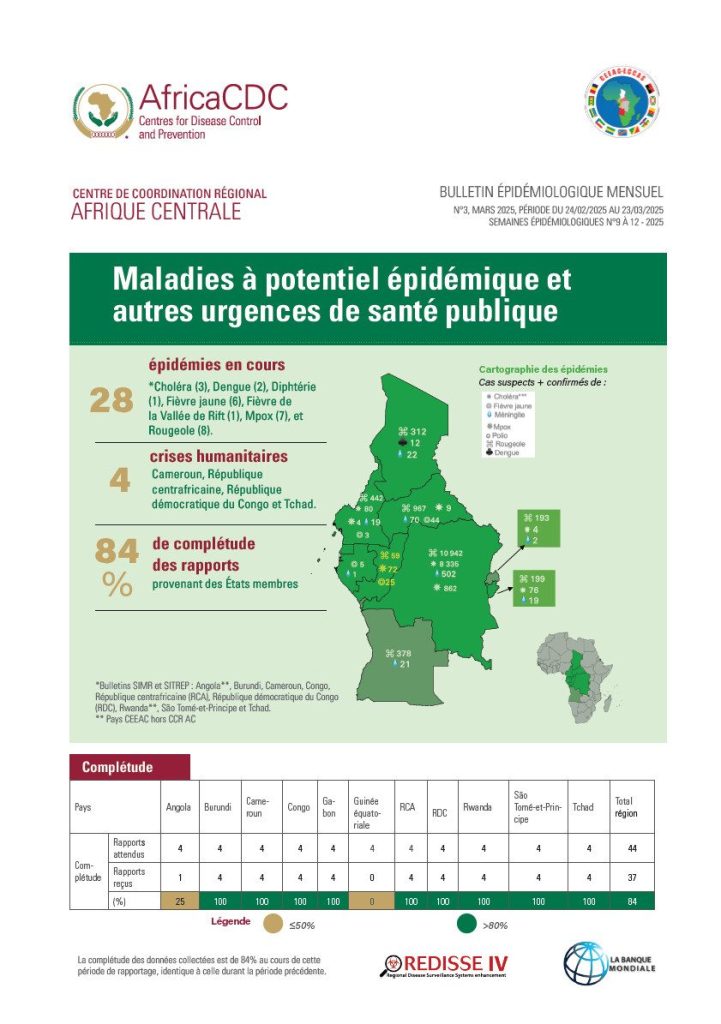
Mpox occurs primarily in tropical rainforest areas of Central and West Africa. The disease is endemic in these regions, with countries like the Democratic Republic of the Congo, Cameroon, and Nigeria frequently reporting cases.
Mpox can spread to humans through close contact with an infected person or animal, or with materials contaminated by the virus, such as clothing, bedding, and towels. Human-to-human transmission occurs primarily through direct skin-to-skin contact, including intimate or sexual contact, and respiratory droplets during sustained face-to-face interaction. The virus can also be transmitted from mother to child during birth or through close contact afterward. Transmission from animals to humans can occur through contact with infected blood, bodily fluids, or lesions.
Symptoms of Mpox include fever, rash, and swollen lymph nodes. The rash typically progresses through several stages: macules, papules, vesicles, pustules, and finally crusting and desquamation over a period of 2 to 3 weeks. Other symptoms can include headache, muscle aches, chills, and exhaustion. The disease is self-limiting, with most people recovering within a few weeks if detected and treated early.
Mpox is usually mild, with most people recovering within a few weeks. However, the severity can vary, with Clade I, found mostly in Central Africa, tending to be more severe than Clade II. Immunosuppressed individuals, such as those with HIV/AIDS, are more vulnerable to severe disease.
Mpox is diagnosed through laboratory testing, specifically using real-time or conventional polymerase chain reaction (PCR) to detect viral DNA in samples collected from skin lesions. Proper specimen collection, handling, and storage are crucial for accurate diagnosis.
There are currently no specific treatments for Mpox. Care focuses on palliative treatment to relieve symptoms and prevent complications. Although not specifically approved for Mpox, antivirals developed for smallpox may offer some benefits, particularly in severe cases or among high-risk individuals.
Yes, vaccines are authorized to prevent Mpox virus infections. Vaccination is recommended for close contacts of confirmed cases and for high-risk populations, including healthcare workers and immunocompromised individuals. The vaccines JYNNEOS (Imvamune or Imvanex) and ACAM2000 are available for preventing Mpox infection.
If you suspect you have Mpox, seek medical attention immediately. Isolate yourself from others to prevent spreading the virus, and follow public health guidance on managing symptoms and preventing transmission.
Prevention of Mpox involves:
- Avoiding close contact with infected individuals or animals.
- Practicing good hygiene, such as regular handwashing and using alcohol-based hand sanitizers.
- Using personal protective equipment (PPE) in healthcare settings.
- Getting vaccinated if you are at high risk or have been exposed to the virus.
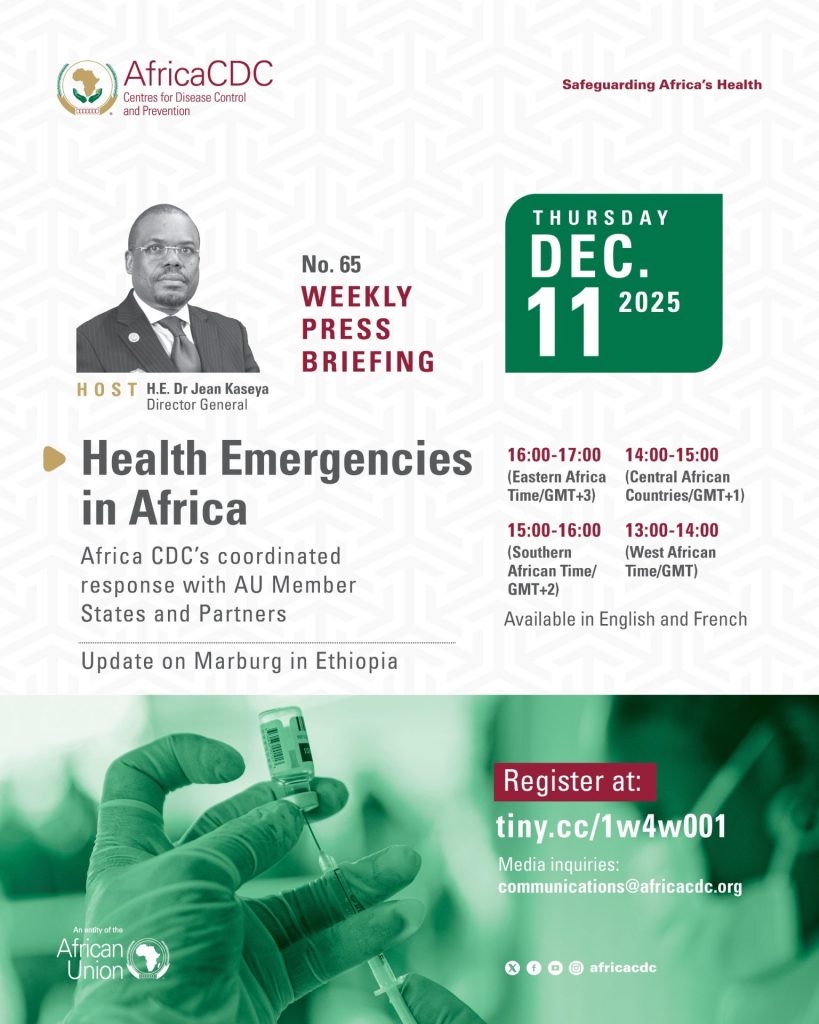
Africa CDC has declared the ongoing Mpox outbreak a Public Health Emergency of Continental Security (PHECS). The agency is mobilizing resources, strengthening surveillance, supporting laboratory testing, and providing technical support to African Union Member States to interrupt the transmission of Mpox across the continent. Efforts include event-based and community surveillance, enhancing laboratory capacities, and coordinating the procurement of vaccines.