Key Facts:
- Monkeypox is a rare, viral zoonotic disease that is caused by the monkeypox virus
- It occurs primarily in tropical rainforest areas of central and west Africa
- Monkeypox can spread in humans through close contact, often skin-to-skin contact, with an infected person or animal, or with material contaminated with the virus such as clothing, bedding, towels
- Signs and symptoms of monkeypox include fever, rash and swollen lymph nodes
- Monkeypox is usually mild, and most people recover within a few weeks
- Diagnostic testing to confirm cases involves using real-time or conventional polymerase chain reaction
- Vaccines developed to protect against smallpox and monkeypox may be used to prevent and treat monkeypox virus infections and antivirals.
What is Monkeypox?
Monkeypox is a rare viral zoonotic disease caused by a double stranded DNA virus that belongs to the Orthopoxvirus genus of the Poxviridae family. The disease presents with symptoms similar to smallpox but with a lesser severity. Monkeypox was first discovered in 1958 when two outbreaks of a pox-like disease occurred in colonies of monkeys kept for research, hence the name ‘monkeypox.’ The first human case of monkeypox was recorded in 1970 in the Democratic Republic of the Congo (DRC), which has subsequently spread to other central and western African countries. There are two known clades of the virus: clade I and clade II. The clade I, which is most frequently reported from countries in central Africa, tends to be more severe than clade II. Cameroon is the only country known to harbour both clades.
Distribution in Africa
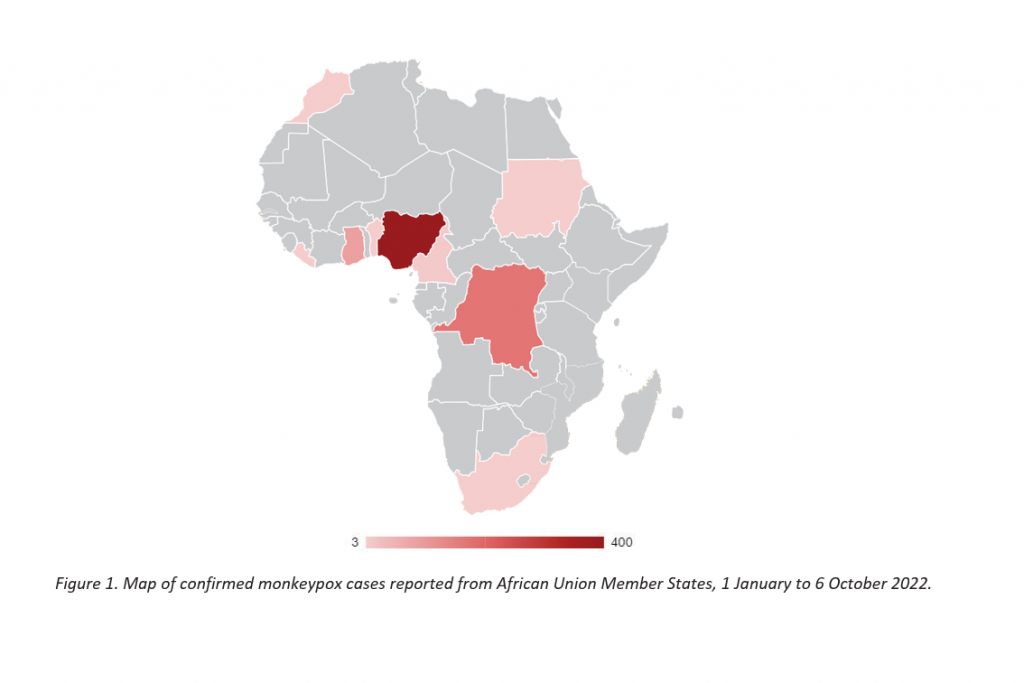
As of October 2022, monkeypox has been reported from 13 Africa Union (AU) Member States (MS): Benin, Cameroon, Central African Republic, Congo, Democratic Republic of the Congo, Egypt, Ghana, Liberia, Morocco, Mozambique, Nigeria, Sudan, and South Africa. Prior to 2022, the following 11 countries have historically reported cases of monkeypox: Benin, Cameroon, Central African Republic, Congo, Côte d’Ivoire, DRC, Gabon, Liberia, Nigeria, Sierra Leone and South Sudan.
Transmission between animals and humans occurs from direct contact with infected blood, bodily fluids, lesions or infected fomites. Person to person transmission mostly is through close contact with respiratory droplets (amplified by sustained face to face contact, skin lesions, and infected fomites as well as mother to child transmission via the placenta or at birth through close contact.
Animal Reservoir Host
Although the transmission cycle of monkeypox is not clearly understood nor has the primary reservoir host of the virus identified, the African rope squirrel (Funisciurus spp.), among other rodent species, is considered a potential reservoir host of the monkeypox virus in endemic regions in Africa.
Clinical Features
Symptoms in humans include fever, headache, muscle ache, chills, exhaustion and swollen lymph nodes. Rash develops within 1 -3 days of infection lasting 2-4 weeks. The disease is self-limiting, and the case fatality rate is between 3-6%. Immunosuppressed individuals are thought to be more vulnerable to severe disease.
Signs in animals are not clearly understood but could include lethargy, lack of appetite, coughing, nasal and/or eye secretions or crust, bloating, fever, and pimple- or blister-like skin rash. A veterinarian should promptly be notified when such symptoms are noticed in animals. Additionally, the index of suspicion should be high if an animal becomes sick within 21 days of contact with a probable or confirmed monkeypox case and should be reported immediately.
Surveillance and Contact Tracing
Surveillance remains a key strategy for early detection of infectious diseases, including monkeypox, and provides a basis on which to respond effectively to an outbreak. Monkeypox surveillance strategies should include early detection of cases, tracing of all close contacts of confirmed cases and protecting high-risk populations to prevent further person-to-person transmission.
Prevention and Control
Infection prevention and control (IPC) measures should be implemented using the One Health approach to break the chain of transmission of monkeypox both in community and healthcare settings.
IPC in Community Settings
The following guidelines should be considered and adopted in community settings:
- Persons with suspected/confirmed monkeypox diagnosis should not leave the home except to seek health care.
- They should avoid contact with wild or domestic animals (if possible)
- Hand washing with soap and water should be performed by infected persons and contacts
- Suspected/confirmed cases of monkeypox should be isolated in a room from other family members where possible
- Persons with monkeypox infection should wear a surgical mask (especially those who have respiratory symptoms e.g., cough, shortness of breath, sore throat) where feasible
- Disposable gloves should be worn to avoid direct contact with lesions, and these should be disposed after each use
- Skin lesions should be covered to the best extent possible (e.g., long sleeves, trousers/long pants) to minimise risk of contact with others
- Laundry (e.g., linen and clothing), dishes and all contaminated surfaces may be washed with hot water, detergent, and disinfectant (0.5% sodium hypochlorite solution)
- The importance of hand hygiene using soap and water, or alcohol-based sanitizer should be emphasised.
IPC for Pet Lovers and Owners
- All pet owners should maintain personal hygiene, such as hand washing with soap and water, and report any suspicious animals to the local veterinary authority
- Anyone infected with monkeypox should avoid contact with animals, especially monkeys, rats, and squirrels
- PPE should be worn by all individuals that care for pets
- Put an end to the use of non-human monkeys in circuses
- Use rodent control measures
Treatment and Care
Many people with monkeypox virus infection have a mild self-limiting disease. There are no specific treatments for monkeypox virus infection currently. However, antivirals developed for the treatment of smallpox may prove to be beneficial against monkeypox. Tecovirimat is approved for the treatment of smallpox in adults and children. It has been shown to decrease the chance of dying, shortens the duration of illness and viral shedding when given in the early course of the disease. Treatment is recommended for people who are severely ill; patients with compromised immune systems like HIV/AIDS patients and people on long term steroids therapy; children, particularly patients younger than 8 years of age; pregnant or breastfeeding women; and people with atopic dermatitis and exfoliative skin conditions. Mental health psychological support services (clinical psychotherapy) should form part of treatment for isolated patients (prior to isolation and during isolation). Assess and monitor for existing mental health ill-health conditions that may worsen during the period of isolation (e.g., anxiety, depression, panic disorders, etc.)
Considerations for special populations People living with HIV
It is currently unknown if HIV increases risk of infection with monkeypox. However, people living with HIV (PLHIV) who are not virally suppressed may be at increased risk of severe morbidity, prolonged illness, and increased mortality. There is no counter-indication for people on pre-exposure prophylaxis who have monkeypox. PLHIV should follow the same recommendations provided in this document to protect themselves from monkeypox. They should also ensure to be adherent to their antiretroviral drug treatment and present for regular follow-ups at their local clinics for continued care.
Vaccination
Vaccination is a known means of prevention against the disease. Africa CDC recommends post- exposure prophylaxis (PEP) with the approved vaccine for all close contacts of a confirmed case. Close contacts include those living in the same household or those who had sex with the case including kissing, hugging and cuddling, sharing of utensils, towels, bedding etc, or came in contact with or touched the rashes on the body of the case3. High-risk populations such as HCWs, immunocompromised individuals and sex workers should also be prioritised for vaccination as mass vaccination is not currently recommended for monkeypox. Two vaccines are available for preventing monkeypox infection: JYNNEOS (Imvamune or Imvanex) and ACAM2000. JYNNEOS is the preferred vaccine for the current outbreak of monkeypox. It is a two-dose vaccine series, administered four weeks apart for maximum effectiveness. A vaccine recipient is considered fully vaccinated two weeks after receiving the second dose. The JYNNEOS vaccine does not cause monkeypox, smallpox, or any significant adverse reaction. Indications for vaccine include known and presume contacts of a case of monkeypox and queer individuals who have had multiple sexual partners in the last 14 days.

