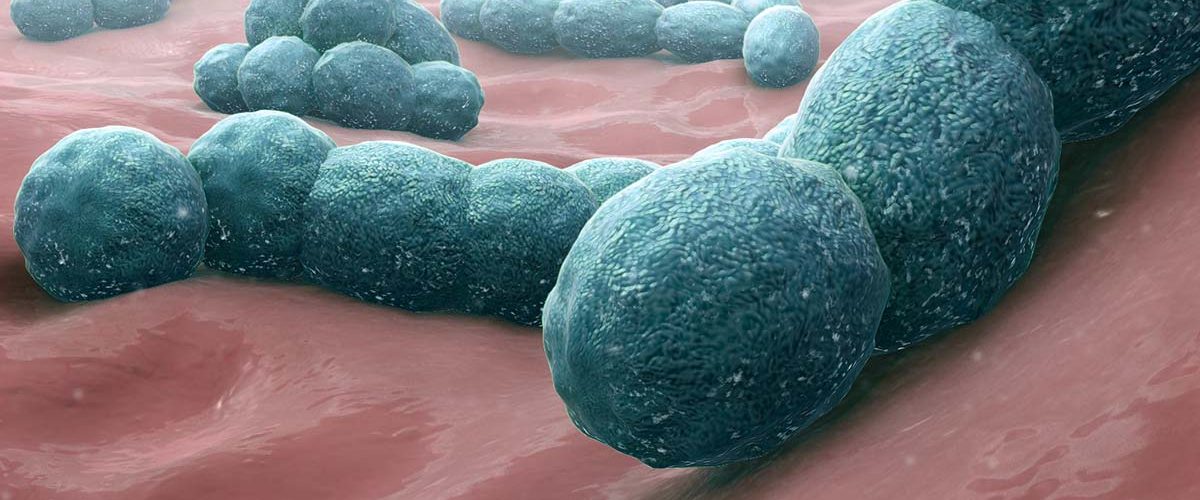
Meningococcal meningitis is a bacterial form of meningitis, a serious infection of the thin lining that surrounds the brain and spinal cord. Meningococcal meningitis is associated with high fatality (up to 50% when untreated). Meningococcal meningitis is observed worldwide but the highest burden of the disease is in the meningitis belt of sub-Saharan Africa, stretching from Senegal in the west to Ethiopia in the east. Around 30 000 cases are still reported each year from that area.
The Neisseria meningitidis bacteria are transmitted from person-to-person through droplets of respiratory or throat secretions from carriers. Smoking, close and prolonged contact – such as kissing, sneezing or coughing on someone, or living in close quarters with a carrier – facilitates the spread of the disease. Transmission of N. meningitidis is facilitated during mass gatherings, For example, the Haj pilgrimage.
The average incubation period is four days , but can range between two and ten days. The most common symptoms are a stiff neck, high fever, sensitivity to light, confusion, headaches and vomiting. A less common but even more severe (often fatal) form of meningococcal disease is meningococcal septicemia, which is characterized by a hemorrhagic rash and rapid circulatory collapse.
Meningococcal disease is potentially fatal and should always be viewed as a medical emergency. Admission to a hospital or health center is necessary. Isolation of the patient is not necessary. Appropriate antibiotic treatment must be started as soon as possible. A range of antibiotics can treat the infection, including penicillin, ampicillin and ceftriaxone. Under epidemic conditions in Africa in areas with limited health infrastructure and resources, ceftriaxone is the drug of choice.
Licensed vaccines against meningococcal disease have been available for more than 40 years. Over time, there have been major improvements in strain coverage and vaccine availability, but to date no universal vaccine against meningococcal disease exists. Vaccines are serogroup specific and confer varying degrees of duration of protection. Meningitis Vaccine are used for prevention (routine immunization) and in response to outbreaks (prompt reactive vaccination). In the African meningitis belt, chemoprophylaxis for close contacts is recommended in non-epidemic situations. Antibiotic prophylaxis for close contacts, when given promptly, decreases the risk of transmission.
Recent Outbreaks in Africa
| Year | Countries | Cases | Deaths |
| 2017 | Liberia | 31 | 13 |
| Nigeria | 1,407 | 211 | |
| Togo | 201 | 17 | |
| 2016 | Togo | 1,975 | 127 |
| 2015 | Nigeria | 652 | 50 |
| Niger | 8,5 | 573 | |
| 2013 | Guinea | 404 | 38 |
| South Sudan | 196 | 13 | |
| 2012 | Benin | 758 | 71 |
| Burkina Faso | 5,3 | 553 | |
| Chad | 2,828 | 135 | |
| Cote d’Ivoire | 399 | 49 | |
| Ghana | 569 | 56 | |
| Sudan | 275 | 13 | |
| 2011 | Chad | 923 | 57 |
| 2010 | Chad | 1,531 | 151 |
| 2009 | Chad | 922 | 105 |
| Nigeria | 17,462 | 960 | |
| Niger | 4,513 | 169 | |
| 2008 | Burkina Faso | 1,422 | 204 |
| DRC | 167 | 17 | |
| Uganda | 380 | 17 |